The Nebraska Department of Veterans Affairs and Department of Health and Human Services are partnering to “Ask the Question” of military service by individuals and family members. The goal is to increase awareness of state and federal benefits and services available to veterans in Nebraska. By doing so, more veterans will be able to connect with resources and services specific to their needs.
The “Ask the Question” Campaign encourages all service providers to ask:
“Have you or a family member ever served in the military?”
This simple question can open the door to greater communication, and communication and understanding is at the heart of good care, services, and connections. Through this insight, it can help to create intentional strategies to better meet the healthcare and community resource needs of Service Members, Veterans, and their families.
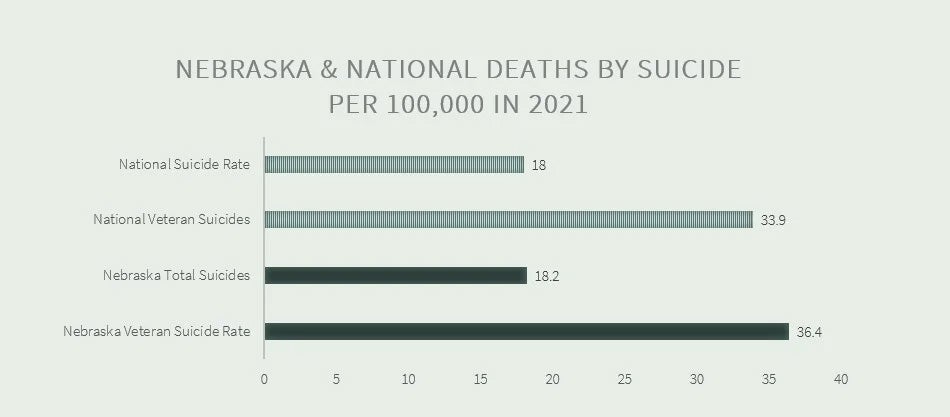
In Nebraska, the suicide rate among veterans was 36.4 per 100,000 individuals, compared to 18.2 per 100,000 deaths by suicide among all Nebraskans in 2021.
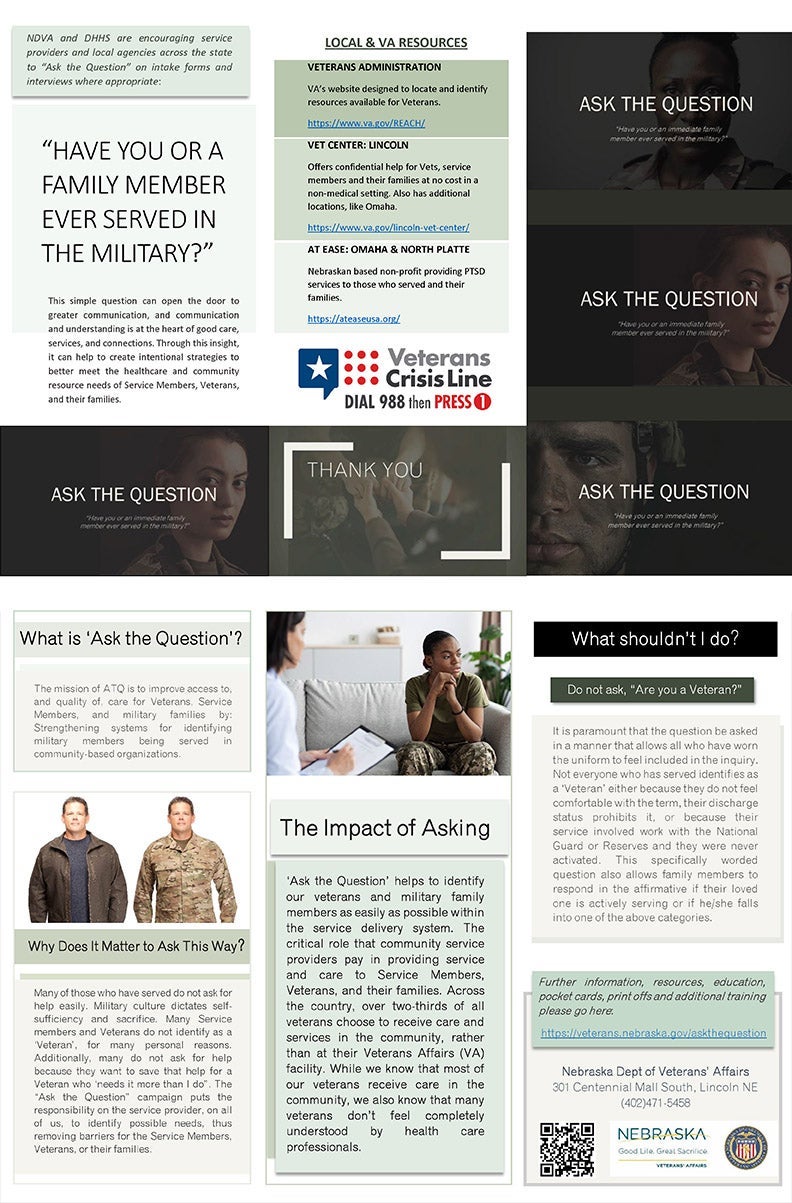
Why Does It Matter to Ask This Way?
Many of those who have served do not ask for help easily. Military culture dictates self-sufficiency and sacrifice. Many Service members and Veterans do not identify as a ‘Veteran’, for many personal reasons. Additionally, many do not ask for help because they want to save that help for a Veteran who ‘needs it more than I do”. The “Ask the Question” campaign puts the responsibility on the service provider, on all of us, to identify possible needs, thus removing barriers for the Service Members, Veterans, or their families.
The Impact of Asking
Ask The Question helps to identify our veterans and military family members as easily as possible within the service delivery system. The critical role that community service providers pay in providing service and care to Service Members, Veterans, and their families. Across the country, over two-thirds of all veterans choose to receive care and services in the community, rather than at their Veterans Affairs (VA) facility. While we know that most of our veterans receive care in the community, we also know that many veterans don’t feel completely understood by health care professionals.
The mission is to improve access to, and quality of, care for Veterans, Service Members, and military families by:
- Strengthening systems for identifying military members being served in community-based organizations.
- Enhancing military cultural competence through education and training of employees, providers, and staff.
- Partnering with civilian-military organization in the community.
The Importance of Educating Leadership, Employees, and Staff
Education about serving Veterans, Service Members and their families is essential to ensure the delivery of high-quality, equitable health care. The vast majority of those who have served receive health care in their communities. Even those who are VA-eligible often choose to access much of their care and services via non-VA resources. Statistically speaking, your facility is already serving Veterans, Service Members and their families. Increasing provider awareness of the unique culture and clinical implications of military service will only improve the quality of the care and services you are already delivering.
Where do I come in?NDVA and DHHS are encouraging service providers and local agencies across the state to “Ask the Question” on intake forms and interviews where appropriate. These include:
|
What shouldn’t I do?Do not ask, “Are you a Veteran?” It is paramount that the question be asked in a manner that allows all who have worn the uniform to feel included in the inquiry. Not everyone who has served identifies as a ‘Veteran’ either because they do not feel comfortable with the term, their discharge status prohibits it, or because their service involved work with the National Guard or Reserves and they were never activated. This specifically worded question also allows family members to respond in the affirmative if their loved one is actively serving or if he/she falls into one of the above categories. |

When the Answer is "Yes"
The following is a series of steps to be taken when encountering an individual who self-identifies as having served in the military. These steps and questions are to be adapted by each facility or organization based on the information needs for the services or care provided. Not all steps or questions will be relevant or appropriate for every program.

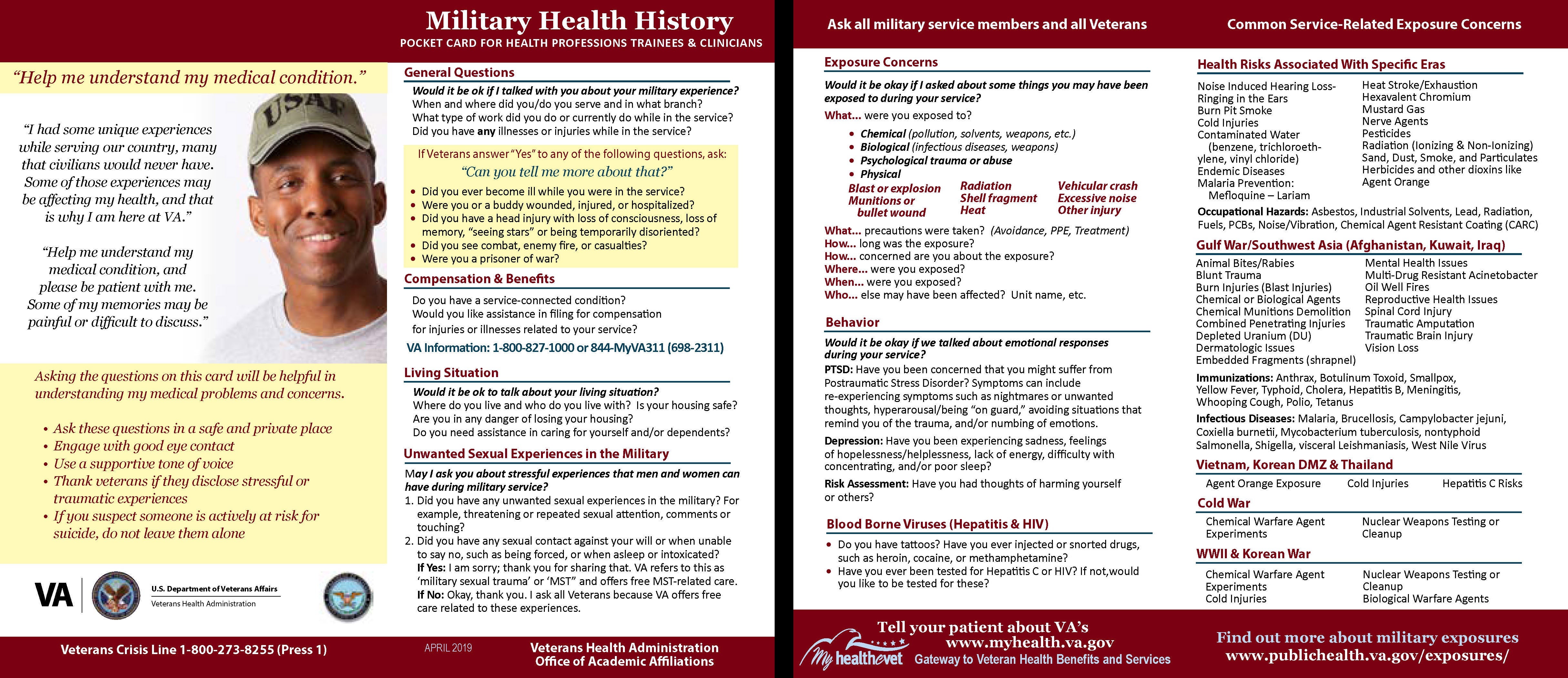
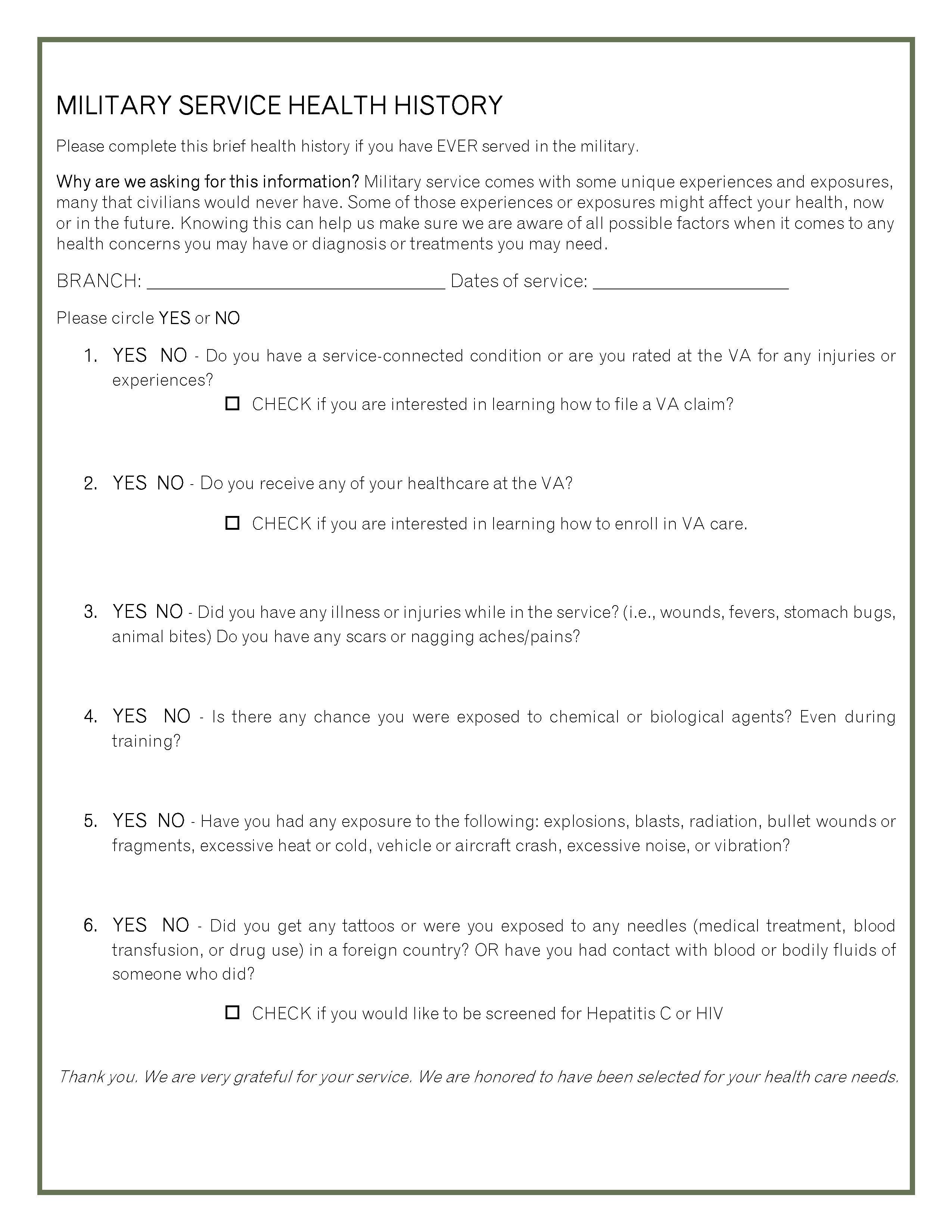
Military Service Health History
When Speaking to a Veteran or Service Member

The following is a series of Steps to be taken when encountering an individual who self-identifies as having served. in the military (Step 1 & 2 can be applied when encountering an individual wearing a service-related hat/shirt/pin, etc.). These steps and questions are to be adapted by each facility or organization based on the information needs for the services or care provided. Not all steps or questions will be relevant or appropriate for every program.
STEP 1
Show appreciation in whichever way you are most comfortable and whichever way seems appropriate for the given situation.
Say: “Awesome!”, “Wonderful!”, “Thank you for your service!”, “Welcome home!”, “You are much appreciated”, “Very cool”.
Eye contact is must, handshakes are optional.
STEP 2
Ask with curiosity and interest: “In which branch did you serve?”, “When did you get out?”, “Which years did you serve?” You might also ask: “What made you choose the [insert Branch served]?” “What was your job?”
If he or she DECLINES to answer your follow questions OR asks, “WHY are you asking me about this?”
Say: “I appreciate your service and am simply curious to know more about you.”
These next steps are intended for care and service level inquiry only. These are not casual questions and should not be asked outside of a professional setting.
STEP 3
Ask: “Do you mind if I ask you a few health-related questions about your military service?”
If he or she DECLINES to answer questions OR asks, “WHY do you need to know about that?”
Say: “Military service comes with unique experiences and exposures, many that civilians would never have. Some of those experiences or exposures might affect your health, now or in the future. Knowing about those things can help me make sure I am aware of all possible factors when it comes to any health concerns you may have or diagnosis or treatments you may need.”
Examples to give if needed:
- breathing problems and chemical or particulate exposures,
- nerve sensitivity concerns and extreme cold exposure,
- memory or concentration issues and exposure to blasts or explosions,
- hearing issues and firearms use or explosions,
- certain unique vaccinations or medical interventions,
- blood borne exposures, or if you received tattoos in a foreign country.
If he or she still DECLINES to answer military-related questions, show your appreciation for their service again and STOP the military health inquiry.
STEP 4
Ask the following series of questions:
- “Do you have a service-connected condition or are you rated for any injuries or experiences at the VA? Do you receive any of your healthcare at the VA?”
- “Did you have any exposure to explosions or blasts? Radiation? Bullet wounds or fragments? Excessive heat or cold exposures? Vehicle or Aircraft Accidents? Excessive noise or vibration?”
“Did you experience any abuse or assaults, combat or otherwise, or any other traumas you want me to know about?”- YES: “Would you like to be screened for PTSD or Depression (at your appointment)?”
- If YES, refer to PCL-5 or PHQ-9.
- “Would you be interested in any information on supports or services that may be available?”
- YES, provide resources handout.
- YES, provide resources handout.
- “Did you get any tattoos or were you exposed to any needles (medical treatment, blood transfusion, or drug use) in a foreign country? Or have you had contact with blood or bodily fluids of someone who did?”
- YES: “Have you ever been screened for Hepatitis C or HIV? Would you like to be?” If YES, arrange for labs or make appropriate medical referral.
Note: If the individual answered YES to any of the above questions, remind him/her that they might qualify for compensation with the VA and offer more information on filing a claim for compensation or refer to a Veterans Services Officer who can assist with filing a claim.
- “Do you have any concerns about your housing?”
- YES: “Would you like information on some supports that may be available?” If YES, provide resources handout.
- YES: “Would you like information on some supports that may be available?” If YES, provide resources handout.
- “Have you ever had thoughts of suicide or homicide?”
- YES: “Are you feeling unsafe today? When was the last time you felt suicidal or homicidal?” If YES, follow your facility/organizational procedure for suicidal or homicidal ideation.
- YES: “Are you feeling unsafe today? When was the last time you felt suicidal or homicidal?” If YES, follow your facility/organizational procedure for suicidal or homicidal ideation.
- “Do you have any concerns about substance use?”
- YES: “Would you like to be screened for a substance use disorder (at your appointment)?” If YES, refer to the ASSIST or AUDIT.
- “Would you be interested in any information on supports or services that may be available?” If YES, provide resources handout.
All YES responses and the relevant details should be recorded in the patient’s Problem List in their medical record so that all medical encounters and associated providers will have the opportunity to consider the impact of the above exposures or needs on any presenting concern.
STEP 5
Thank the individual again for his/her service and remind them that you are honored they chose your facility for their health care needs.
Concerned for a Veterans' Safety?
Resources for Providers
Military Health History
Pocket Card for Health Professions, Trainings, and Clinicians
"Ask the Question" Toolkit
Print-friendly reference guide to ATQ
"Ask the Question" Breakroom Poster
Please consider hanging this in locations for quick reference for staff.
"Ask the Question" Trifold
Please have available to provide for reference of staff, veterans, their families, and the general public.
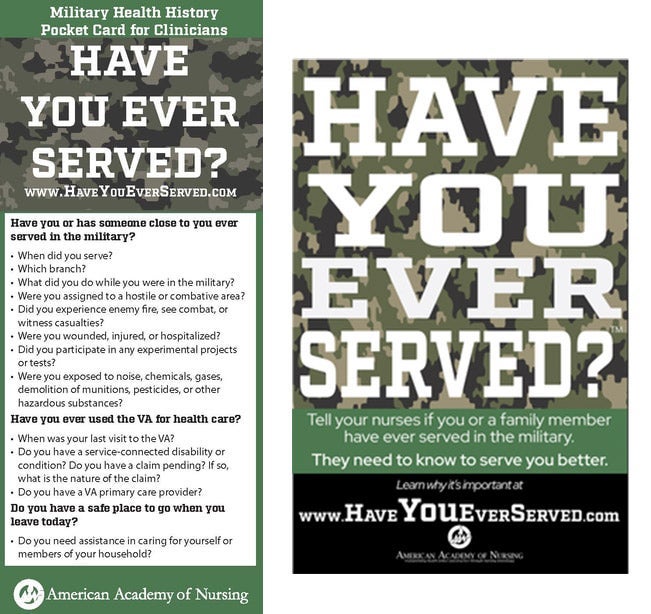
Have You Ever Served?
A helpful, quick reference pocket card and poster of questions to ask for better understand a veteran’s military health history, designed specifically for physicians and health professionals.
Additional Resources
Veterans Administration Provided Resources
- VA/NC-PTSD Community Provider Toolkit - A resource for healthcare professionals working with veterans outside of the VA health care system with information and tools relevant to veterans’ mental health and well-being curated especially for community providers.
- Veterans Health Administration TRAIN Courses for Providers - The most comprehensive catalog of public health training opportunities. Note: it does require an account creation to utilize. TRAIN is a free service for learners from the Public Health Foundation. VHA TRAIN is supported by the Veterans Health Administration Institute for Learning, Education and Development (ILEAD), an internal education and training program office in the Department of Veterans Affairs. The ILEAD-developed learning programs found in VHA support the professional development needs of public health and health care providers, with a focus on Veteran patient care.
SAMHSA Provided Resources
- Stanley Brown Safety Plan - Video and webinar resources for healthcare clinicians including a Safety Planning Webinar with demonstration videos and a brief example of essential aspects of the Safety Planning Intervention.
- Columbia-Suicide Severity Rating Scale Risk Assessment (C-SSRS) - The C-SSRS is the most evidence-supported tool of its kind, is a simple series of questions that anyone can use anywhere in the world to prevent suicide.
- PHQ9 Depression Scale - A multipurpose instrument for screening, diagnosing, monitoring, and measuring the severity of depression. The PHQ-9 incorporates DSM-IV depression diagnostic criteria with other leading major depressive symptoms into a brief self-report tool.


 Save or print this questionnaire as a PDF.
Save or print this questionnaire as a PDF.